Connect With Us
Blog

Symptoms and Risks for Ball of Foot Pain

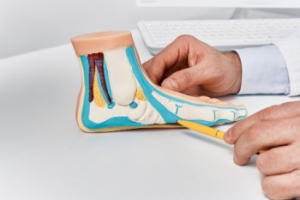
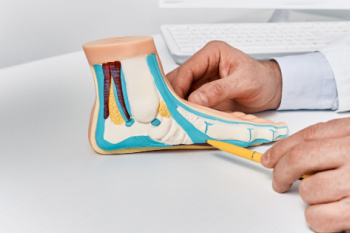
Ball of the foot pain, medically known as metatarsalgia, often develops gradually and affects the area between the arch and toes, particularly around the metatarsal bones. Common symptoms of ball of the foot pain include a sharp, burning pain or the sensation of stepping on small stones. Some patients also experience numbness or tingling in the toes. Symptoms typically intensify with prolonged standing, walking, running, or when participating in high-impact sports like jumping. Wearing ill-fitting footwear, especially shoes that are too tight, too loose, or lack proper cushioning, can significantly contribute to discomfort. High heels frequently shift extra weight onto the front of the foot, further aggravating symptoms. Additionally, foot abnormalities such as high arches, longer second toes, bunions, or hammertoes increase susceptibility. For persistent discomfort, a podiatrist can assess your condition, perform diagnostic tests like X-rays or MRI scans, and provide customized treatment options, potentially including orthotics or surgery. If you experience ongoing pain in the ball of your foot, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Hoover, Oneonta, and Munford, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Facts About Gout Attacks

Gout is a form of arthritis caused by the buildup of uric acid crystals in the joints, leading to sudden and intense pain. This condition commonly affects the big toe but can also involve other joints such as the ankles, knees, and wrists. Uric acid accumulates when the body produces too much of it or fails to eliminate it efficiently. Consuming foods high in purines, such as red meat and seafood, excessive alcohol intake, obesity, and certain medical conditions can contribute to the development of gout. Symptoms include severe joint pain, redness, swelling, and warmth in the affected area. Episodes often occur unexpectedly and may last for several days. If you have developed this painful condition, it is suggested that you are under the care of a podiatrist who can help you to manage gout.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in Hoover, Oneonta, and Munford, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Gout
Gout is a form of arthritis that is caused by a buildup of uric acid crystals in the joints. This considered to be one of the most frequently recorded medical illnesses throughout history. Gout occurrences in the US have risen within the past twenty years and the condition now affects 8.3 million people which is 4% of all Americans. Researchers have found that gout affects men more than women and African-American men more than white men.
Symptoms of gout are warmth, swelling, discoloration, and tenderness in the affected joint area. The small joint on the big toe is the most common place for a gout attack to occur.
People who are obese, gain weight excessively, drink alcohol heavily, have high blood pressure, or have abnormal kidney function are more likely to develop gout. Furthermore, certain drugs and diseases are likely to increase levels of uric acid in the joints which eventually leads to gout. You are also more likely to develop gout if you eat a lot of meat and fish.
Many who experience gout attacks will experience repeated attacks over the years. Some people who have gout symptoms, may never have them again, but others may experience them several times a year. If you have gout symptoms throughout the year, you may have recurrent gout. Those who have gout should also be careful about their urate crystals collecting in their urinary tract, because this may lead to kidney stones.
Diagnosis for gout is done by checking the level of uric acid in the joints and blood. Your podiatrist may also prescribe medicine to reduce uric acid buildup in the blood, which will help prevent any gout attacks.
To treat gout, your podiatrist may also prescribe you Anti-inflammatory medication (NSAIDs) which will relieve the pain and swelling of a gout episode and it can also shorten a gout attack. Maintaining a healthy diet is also a proven method to prevent gout attacks.
Reasons Why Ankles May Hurt After Cycling

Cycling, while a low-impact activity, can still lead to various ankle injuries. Achilles tendinitis is a frequent issue, caused by overuse or wearing improper footwear, leading to pain and inflammation in the Achilles tendon. Plantar fasciitis, another common condition, results from repetitive stress on the foot arch, causing heel pain. Metatarsalgia involves pain in the ball of the foot, often caused by poor bike fit or pressure on the toes. Numbness in the feet can also occur, often due to prolonged pressure or improper foot positioning. Ankle sprains, typically caused by sudden twists or improper bike handling, can result in ligament damage. Additionally, fractures may occur from falls or accidents, particularly if the ankle is subjected to forceful impact. If you have ankle pain while cycling, it is suggested that you consult a podiatrist who can effectively treat such conditions.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact our office located in Hoover, Oneonta, and Munford, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.
Signs of Peripheral Neuropathy in the Feet

Peripheral neuropathy in the feet can develop slowly, causing various noticeable symptoms. One of the most common signs is a gradual numbness, making it difficult to feel sensations in the feet. People with this condition may also experience increased sensitivity to touch, where even light pressure or a slight tap can cause discomfort. A lack of coordination is another symptom, often leading to difficulty walking or maintaining balance. Sharp or throbbing pain can also be present, especially at night or after long periods of standing or walking. Muscle weakness is another indication of peripheral neuropathy, as the feet may feel heavy or less responsive during movement. If left untreated, these symptoms can worsen over time, affecting daily activities and overall quality of life. If you have signs of peripheral neuropathy in the feet, it is suggested that you consult a podiatrist who can help you to manage this condition.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Hoover, Oneonta, and Munford, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Facts About Flat Feet
Flat feet, or pes planus, occur when the arches of the feet are absent, causing the entire sole to make contact with the ground. This condition is common among infants and toddlers, but typically resolves as the tendons and ligaments strengthen during early childhood. For some people, flat feet persist into adulthood or develop later due to injuries, aging, or conditions such as posterior tibial tendon dysfunction. Symptoms can range from no discomfort to pain in the feet, ankles, or lower legs, especially after prolonged standing or physical activity. Tight Achilles tendons and damage to the tendons that support the arch can contribute to flat feet, making walking and running uncomfortable. In cases where flat feet lead to significant pain or mobility issues, a podiatrist can use imaging tests and physical assessments to assess the severity. Treatment may include custom orthotics, shoe modifications, or in severe cases, surgery to repair or support the foot’s structure. If you have foot problems related to flat feet, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Hoover, Oneonta, and Munford, AL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- October 2025
- September 2025
- August 2025
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023