Connect With Us
Blog

Types of Toenail Fungus

Toenail fungus, medically termed onychomycosis or tinea unguium, is a common fungal infection that affects approximately 14 percent of people, as reported by the Centers for Disease Control and Prevention. While typically not a serious health concern, toenail fungus can cause cosmetic issues as well as discomfort. There are various types of toenail fungus, each with distinct characteristics in symptoms and appearance. The most prevalent form is subungual onychomycosis, characterized by nail lifting, discoloration, and crumbling of the toenail. White superficial onychomycosis causes white, flaky patches on the nail surface, potentially progressing to rough and crumbly nails. Candida onychomycosis, caused by yeast, is more common in individuals with conditions like diabetes or compromised immune systems. This type of toenail fungus shows symptoms such as rough nails, surface breakdown, and soft tissue infection. An accurate diagnosis by a podiatrist is essential to determine the type of toenail fungus you may have incurred. With proper care and timely intervention, toenail fungus can be effectively managed. If you suspect you have a toenail fungus, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options appropriate to the cause.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Charles Oehrlein, DPM of Hoover Foot Care. Our practitioner can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Hoover, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
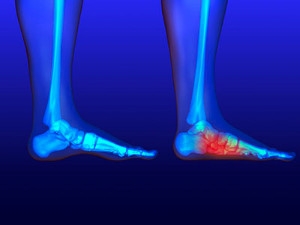
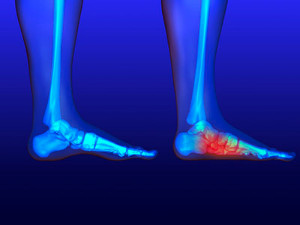
Causes of Bone Spurs on the Heel

Heel bone spurs, medically known as osteophytes, are abnormal growths that can result in pain and restricted movement. Often unnoticed until visible on an X-ray, heel bone spurs are associated with degenerative joint diseases, such as osteoarthritis, where the breakdown of joint cartilage prompts the body to form new bone as a reparative measure. This process leads to the development of bone spurs along the edges of affected joints, particularly in the heel region. Besides aging, various factors contribute to heel bone spurs, including injuries and overuse, common among runners and dancers. Other factors are hereditary predisposition, obesity, and congenital bone issues. Many people may have heel bone spurs without symptoms, but others can experience pain and loss of joint mobility if the spur rubs against bones or presses on a nerve. If you suspect you have a heel bone spur or are experiencing unexplained heel pain, it is suggested that you schedule an appointment with a podiatrist for a comprehensive evaluation and the appropriate treatment plan.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Hoover, AL . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Diagnosis and Management of Flat Feet
Pes planus, commonly known as flat foot, is a condition where the arch of the foot is lower or in contact with the ground when compared to the typical foot structure. It is important to note that infants are born with flexible flat feet. Arch development usually begins at approximately 3 years of age, and reaches adult levels in arch height between 7 and 10 years old. Flexible flat feet can be developmental in infants and toddlers but may be considered true flat feet by age 8 to 10. On the other hand, rigid flat feet are associated with underlying pathology and lack the longitudinal arches both in heel elevation and weight bearing. Acquired flat feet can develop from various factors, particularly diabetes, which can affect the structure and functionality of the feet. Additionally, foot and ankle injuries can lead to the development of flat feet. Certain medical conditions, including arthritis, spina bifida, cerebral palsy, and muscular dystrophy, are also associated with acquired pes planus. Interestingly, pregnancy can be a factor in the development of flat feet due to the changes that occur in the body during this period. Regardless of the reason for your flat feet, if they are causing you problems, it is suggested that you schedule an appointment with a podiatrist who can help you to find relief.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Hoover, AL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
Occupational Hazards of Plantar Fasciitis

Plantar fasciitis is prevalent in manufacturing environments, with several factors influencing its occurrence. These can include forefoot pronation during physical examination, high metatarsal pressure in gait assessments, and prolonged standing on hard surfaces. The rotation of footwear during the workweek appears to reduce the likelihood of developing plantar fasciitis. Using shoe orthoses with medial longitudinal arch and metatarsal pads can serve as a preventive or treatment approach. Implementing workstations that reduce the time spent walking or standing on hard surfaces, such as offering cushioning mats or alternating sitting and standing postures, may help lower the risk of plantar fasciitis. If you work in manufacturing and have developed heel pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis, treatment, and additional preventative advice.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Hoover, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Foot Stretches for Graceful Toe Point

Achieving a beautifully pointed toe is a hallmark of grace in ballet, and dedicated foot stretches can significantly contribute to this desired aesthetic. Begin by sitting with your legs extended and gently flex and point your toes, emphasizing the extension of each digit. A towel stretch proves effective, which is done by looping a towel around the ball of your foot and gently pulling it towards you, feeling the stretch along the arch and toes. Rolling a tennis ball beneath the arches and toes massages and improves flexibility. Additionally, the seated toe stretch involves sitting back on your heels, elongating the toes, and fostering a deep stretch. Practicing these stretches regularly enhances the flexibility and strength of the foot's intrinsic muscles, contributing to a more refined toe point. Incorporating these targeted stretches into your ballet warm-up or cool-down routine can cultivate the suppleness necessary for achieving that coveted, elegant toe point on stage. If you would like additional information about effective foot and toe stretches, it is suggested that you confer with a podiatrist.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Charles Oehrlein, DPM from Hoover Foot Care. Our practitioner will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
- Using a foam roller or any cylindrical object (a water bottle or soda can will do), roll the object under your foot back and forth. You should also exert pressure on the object. Be sure to do this to both feet for a minute. Do this exercise three times each.
- Similar to the previous one, take a ball, such as a tennis ball, and roll it under your foot while seated and exert pressure on it.
- Grab a resistance band or towel and take a seat. If you are using a towel, fold it length wise. Next put either one between the ball of your foot and heel and pull with both hands on each side towards you. Hold this for 15 seconds and then switch feet. Do this three times for each foot.
- Finally hold your big toe while crossing one leg over the other. Pull the toe towards you and hold for 15 seconds. Once again do this three times per foot.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising and ice and rest the foot. It is advised to then see a podiatrist for help.
If you have any questions, please feel free to contact our office located in Hoover, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Stretch Your Feet
Your feet endure a great amount of stress each day from constantly allowing us to move around. It is important to stretch your feet to help prevent them from becoming injured. Your toes may easily deform into unhealthful positions if they are not stretched.
One of the most common reasons for toe deformities are the shoes you may be wearing. Shoes that are too tight may fold and shift the toes out of place. Heeled shoes may also push your toes upward. Forcing your toes into an unnatural position which may cause the muscles to tighten and prevent them from reverting to normal length. Another common reason is improper use of foot muscles. Many people fail to use the muscles in their feet or toes when they walk. Lastly, the positioning of your feet while walking may also cause toe deformities. If you walk with your feet facing outward, your “push-off” phase is on the side of your big toe instead of the bottom of your foot. This may cause the big toe to eventually tighten into a new shifted position.
There are many reasons why stretching your toes may be helpful. One reason is that healthy spacing may aid in avoiding calluses and other injuries that are caused by rubbing. Stretching will also prevent you from developing toes that curl, hammertoes, or bunions.
A great way to stretch your toes is to place them in your hands and bend them all downward; this will help you stretch the top of your foot. Next, you should repeat this process but instead bend them upward enough to feel a nice stretch in the bottom of your foot. You should then try to pull each toe apart from the next and pull any toes that are bent upward until they are back downward.
If you are looking to practice stretching your entire foot, you can try a towel stretch. This is done by sitting on the floor with your legs in front of you. Take a towel and wrap it around your toes. Afterward, pull the towel toward you with your toes and hold this position for 15 to 30 seconds before releasing. Practice this stretch for three sets. Another stretch your feet are towel lifts. This is done by sitting in a chair and trying to pick a towel up from the ground with your toes. Try lifting the towel with your little toes for five sets before switching feet.
If you are an athlete, or exercise often, it is especially important for you to practice stretching your feet. Those who suffer from foot pain caused by poor footwear, plantar fasciitis, or long hours of standing at work may also benefit from foot exercises.
Blog Archives
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023